Vertex: 83% of patients completely free from insulin dependence! Stem cell therapy is expected to completely "end" diabetes
Diabetes is a chronic metabolic disease with multiple complications, significant harm, and a trend of affecting younger populations. It can be mainly divided into two major types: type 1 and type 2. Type 1 diabetes is an autoimmune disease, accounting for about 5-10% of total cases, and it primarily occurs in children. Type 2 diabetes accounts for about 90% of cases, often associated with lifestyle factors such as obesity and sedentary behavior. Although it is more common in middle-aged and elderly people, the age of onset has gradually shifted to younger populations in recent years.
According to the International Diabetes Federation (IDF) data, the number of adults with diabetes worldwide reached 589 million in 2024 (accounting for 11.1%, equivalent to approximately 1 in every 9 people having diabetes). It is estimated that by 2050, the total number of adults with diabetes worldwide will increase to 853 million (accounting for 13.0%). China has the highest number of diabetes patients in the world.
In recent years, stem cell technology has shown great application prospects in the field of diabetes treatment. Many breakthrough advancements have brought new hope to the treatment of diabetes, promising to fundamentally change its treatment paradigm.
83% of patients have completely overcome their insulin dependency, and the product is about to be submitted for market approval
Recently, Vertex Pharmaceuticals (hereinafter referred to as "Vertex") announced Phase 1/2 breakthrough clinical research data for its stem cell therapy, zimislecel (formerly VX-880), for the treatment of type 1 diabetes at the 85th Scientific Sessions of the American Diabetes Association (ADA).
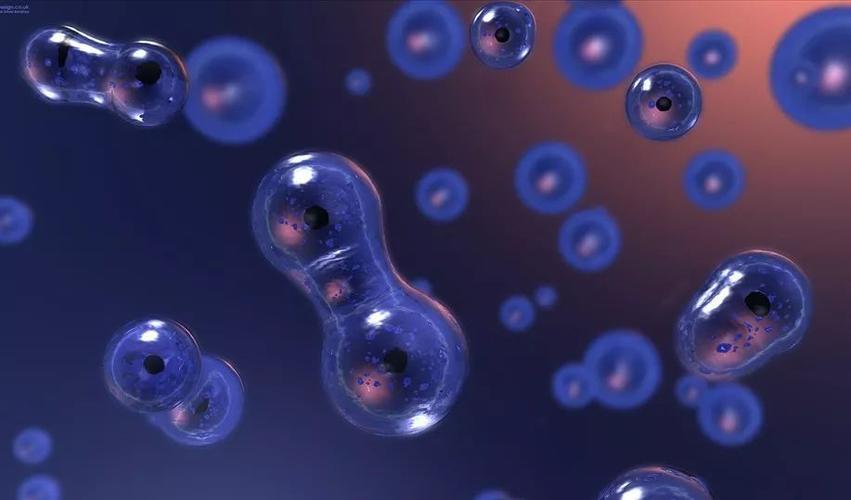
Zimislecel is a fully differentiated insulin-producing islet cell therapy derived from allogeneic stem cells, currently under research at Vertex. This therapy holds promise for restoring the body's ability to regulate glucose levels by restoring islet cell function, including glucose-responsive insulin production.
According to the disclosed information, 83% (10/12) of the patients completely got rid of insulin dependence after one year of injection and stopped experiencing episodes of hypoglycemia, which can lead to dangerous complications and even death. The relevant data has been simultaneously published in the New England Journal of Medicine (NEJM).
Specifically, in terms of efficacy, all 12 patients who received treatment achieved the ADA-set targets of glycated hemoglobin (HbA1c) <7% and target-in-range (TIR) >70% for blood glucose; and from day 90 onwards, there were no severe hypoglycemic events (SHE), meeting the primary endpoint of the Phase 1/2 clinical trial.
Furthermore, patients exhibited a significant reduction in exogenous insulin usage, with an average daily insulin dose decreasing by 92%. Regarding insulin secretion recovery, C-peptide levels, a biomarker closely associated with insulin secretion, were detected in all patients following infusion. The same recovery of C-peptide levels was also observed in another group of patients receiving lower doses of treatment.
In terms of safety, Zimislecel has demonstrated good overall tolerability. No serious adverse events related to Zimislecel treatment have been observed, and the two reported deaths of patients were unrelated to Zimislecel treatment.
Dr. Trevor Reichman, a researcher involved in the trial and from the University Health Network in Toronto, stated that this is the first time artificial stem cell "islets" have enabled such a high proportion of patients to become insulin-independent. This holds promise for addressing the long-standing challenge of limited organ donations, providing an "almost unlimited supply" of islet cells for future treatments.
Although Zimislecel currently requires long-term immunosuppressive therapy to protect islet cells from immune rejection, Vertex has been seeking to develop stem cells that do not require immunosuppression, potentially by genetically engineering or encapsulating the cells to make them "invisible" to immune attack. However, it is worth noting that in March this year, Vertex's VX-264 therapy, which aims to avoid immunosuppression through islet cell encapsulation technology, failed in Phase 1/2 clinical trials.
Currently, Zimislecel is the only diabetes stem cell therapy being developed by Vertex, and it has entered Phase 3 clinical trials. If the data continues to be positive, Vertex plans to submit an application for marketing authorization in 2026.
The global race for diabetes stem cell pipelines is underway, with multiple technological paths advancing simultaneously
In recent years, the global pipeline of diabetes stem cell therapies has accelerated, covering both type 1 and type 2 diabetes. From a technological perspective, stem cell therapy for diabetes mainly focuses on two directions: cell replacement, paracrine signaling, and immune regulation, with the goal of achieving a "functional cure".
The specific strategies of the cell replacement pathway include pluripotent stem cell differentiation, tissue and organ cell reprogramming, and the generation of islet-like organs from pancreatic islet adult stem cells. Pluripotent stem cells (including embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs)) can restore physiological insulin secretion by differentiating into pancreatic β cells. This pathway, represented by Vertex's zimislecel, can overcome the limitation of donor shortage.
Reprogramming technology is also one of the current research hotspots. Taking chemical reprogramming as an example, in September 2024, Deng Hongkui's team from Peking University published a paper in the internationally authoritative journal Cell, claiming to have achieved the first clinical functional cure for type 1 diabetes patients by utilizing chemical reprogramming technology to prepare islet cells. By reprogramming and transdifferentiating somatic cells into islet cells to replace the dysfunctional islet cells in patients' bodies, long-term stable control of blood glucose levels was achieved.
Starting from 75 days after treatment, the patient regained endogenous and autonomous glucose regulation ability, and ultimately completely discontinued insulin injection therapy. As of the time of paper publication, the patient had been insulin-free for over a year, and the blood glucose compliance rate had continuously increased from a baseline of 43.18% to over 98%, remaining stable.
Its partner company, Hangzhou Ruipu Chentuang, also received clinical approval for its RGB-5088 islet cell injection in December last year, making it the first pluripotent stem cell product in China to be approved for clinical use in the treatment of type 1 diabetes.
Professor Yin Hao's team from Shanghai Changzheng Hospital, in collaboration with Professor Cheng Xin's team from the Center for Excellence in Molecular and Cellular Biosciences of the Chinese Academy of Sciences, utilized cell reprogramming and directed differentiation techniques to convert blood cells from healthy donors into endoderm stem cells (EnSCs). These EnSCs were then used to generate regenerative islets (E-islet 01), which exhibit structures and functions consistent with healthy islets.
In April this year, E-islet 01 received clinical approval in China, becoming the first allogeneic universal regenerative islet product in the country and the second globally to enter the clinical trial phase. Public information shows that E-islet 01 has successfully functionally cured multiple patients with type 1 and type 2 diabetes.
Mesenchymal stromal cells (MSCs) are also a research direction in diabetic cell therapy, but most of the focus is on type 2 diabetes. MSCs do not directly differentiate into pancreatic islet cells, but indirectly improve the pancreatic islet environment by secreting anti-inflammatory factors and regulating the immune microenvironment, thereby exerting a protective effect on endogenous pancreatic islets.
The human adipose stem cell injection with high expression of both GLP-1 (gut-derived polypeptide) and FGF21 (liver-secreted cytokine), independently developed by Jiyuan Biotechnology, is the first gene-modified stem cell approved for clinical use in China, intended for the treatment of refractory type 2 diabetes. The research team innovatively utilized gene technology to fuse GLP-1 and FGF21 with adipose MSCs, developing a CAR-Like MSC capable of synergistically targeting and regulating abnormal glucose and lipid metabolism. It not only achieves dual-factor regulation of glucose and lipid metabolism but also utilizes homing characteristics to achieve targeted local treatment, exerting the efficacy of protecting pancreatic β cells and inhibiting complications.
Dabuo Biotech's E10I human umbilical cord mesenchymal stem cell injection, which is also intended for type 2 diabetes, received clinical approval in March this year. In early non-registered clinical studies, E10I demonstrated a significant trend towards lowering blood sugar and reducing inflammation, without any serious adverse events.
Conclusion:
The functional cure of diabetes has always been a major challenge in the field of regenerative medicine. Stem cell therapy is regarded as one of the most promising methods for treating diabetes. Globally, diabetic stem cell therapy has shown a trend of multiple technological paths advancing simultaneously.
Although some technologies still need to overcome key bottlenecks such as long-term safety, the progress of diabetes stem cell therapy globally is accelerating with the iteration of technologies and the cross-integration of multiple technological paths. This will also strongly promote the continuous progress and development of the regenerative medicine field.